Acute Ischemic Stroke
Acute Ischemic Stroke (AIS) affects millions of individuals worldwide, with a significant impact on mortality and disability rates. According to the World Health Organization, it is a leading cause of death and disability globally, making effective interventions crucial to reducing its impact.
More About This Condition
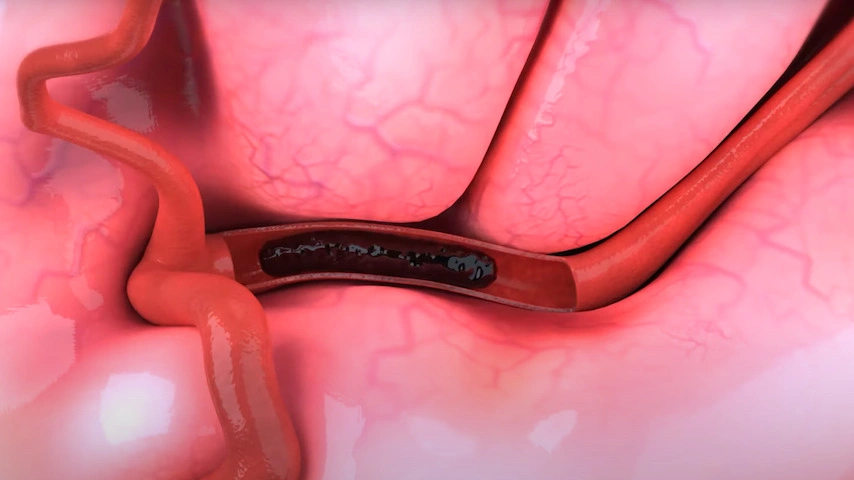
The brain depends on a constant supply of blood for the oxygen and nutrients it needs to survive. Pipe-like vessels called arteries carry oxygenated blood from the heart and lungs to all parts of the brain. AIS can occur when blood flow through one of these arteries is blocked. Stroke robs the brain of oxygen, causing brain cells to become damaged or die. As a result, parts of the body controlled by those cells often become disabled.
Ischemic stroke represents 87% of all strokes. A large vessel occlusion is a severe and debilitating type of ischemic stroke as the clot occludes major arteries and prevents blood flow to significant portions of the brain.
IMPORTANT NOTE: This overview is provided for informational purposes only and should not be used as a substitute for talking with your doctor. Be sure to talk with your doctor for a complete discussion of this condition as well as the benefits and risks of any treatment options.
Symptoms
All stroke types can cause serious, sometimes fatal, complications. Stroke symptoms can vary from person to person depending on stroke type and location in the brain. The acronym BE FAST (Balance, Eyes, Face, Arm, Speech, Time) has been popularized in the United States and elsewhere to teach the telltale signs of stroke and the critical need to contact emergency services immediately. Difficulties with balance, blurred vision, face drooping, arm weakness, and speech difficulty are the outward signs that it’s time to call 911.
Symptoms may include:
- Sudden weakness
- Sudden confusion
- Vision problems
- Trouble speaking or understanding speech
- Trouble walking, loss of balance, dizziness, or lack of coordination
- Paralysis or numbness of the face, arm, or leg
Diagnosis
Your doctor may:
- Ask you or your family member about your risk factors, such as high blood pressure, smoking, heart disease, and a personal or family history of stroke.
- Ask about your signs and symptoms and when they began.
- Conduct a physical examination to assess your mental alertness, coordination, and balance.
Your doctor may order one or more of the following tests:
- Computed tomography (CT) scan involves the use of a special X-ray scanner and a computer to create many two-dimensional images, or “slices” of the brain that can be stacked to create a detailed picture.
- Magnetic resonance imaging (MRI) uses computer-generated radio waves and a magnetic field to create two- and three-dimensional detailed images of the brain.
- Catheter-based angiography involves an injection of contrast dye into the arteries. The dye is injected via a catheter, a long tube-like device that is inserted into a leg or arm artery and slowly threaded through the body up to the neck. The dye helps create a detailed image of the arteries on an X-ray in two or three dimensions.
Treatment
Treatment for this condition must always be discussed with your doctor for a full discussion of options, risks, benefits, and other information.
Medical treatments available to acute ischemic stroke patients have advanced by leaps and bounds since they were first introduced in the 1990s. Today’s innovative technologies and techniques can remove clot and restore blood flow through the brain more effectively and in less time than ever before.
Swift medical treatment is needed because the brain relies on a constant supply of blood for the oxygen and nutrients it needs to survive. When circulation through a blood vessel is blocked, brain cells nearest the occlusion may become damaged or die. Restoring blood flow within the first hours of symptom onset is crucial to achieving positive patient outcomes.
Treatment Procedures Include:
Mechanical thrombectomy is an endovascular procedure that uses a thin tube-like device called a catheter to clear blocked arteries and restore blood flow.
- Catheters use suction or deploy a stent retriever to remove clot. Sometimes both approaches are used during a single procedure.
- Catheters are inserted into a leg artery and slowly threaded through the body up to the blocked vessel in the brain.
- Mechanical thrombectomy should be performed as soon as possible after symptom onset.
Tissue plasminogen activator (tPA), a clot-busting drug, is another option used to treat stroke and is often used prior to mechanical thrombectomy. tPA, infused into a vein, works by dissolving the clot.
- tPA needs to be used as quickly as possible, typically within a five-hour window in certain eligible patients of symptom onset.
- tPA often fails to completely dissolve blood clots in larger arteries.
- Not all patients are eligible to receive tPA.
Mechanical thrombectomy may be the only option for a significant segment of the AIS patient population, including patients who either miss the window to receive tPA and/or have large vessel occlusions for which thrombolysis has limited efficacy. Other patients benefit from a combination of intravenous and endovascular treatments. Increasingly, practitioners are taking advantage of the benefits of each type of intervention to help save patients from irreversible brain damage.
Learn More
